Donanemab (KISUNLA) FDA-approved for Alzheimer's: Should we recommend it?
- Jason Cafer MD
- Jul 9, 2024
- 8 min read
Updated: Jul 11, 2024
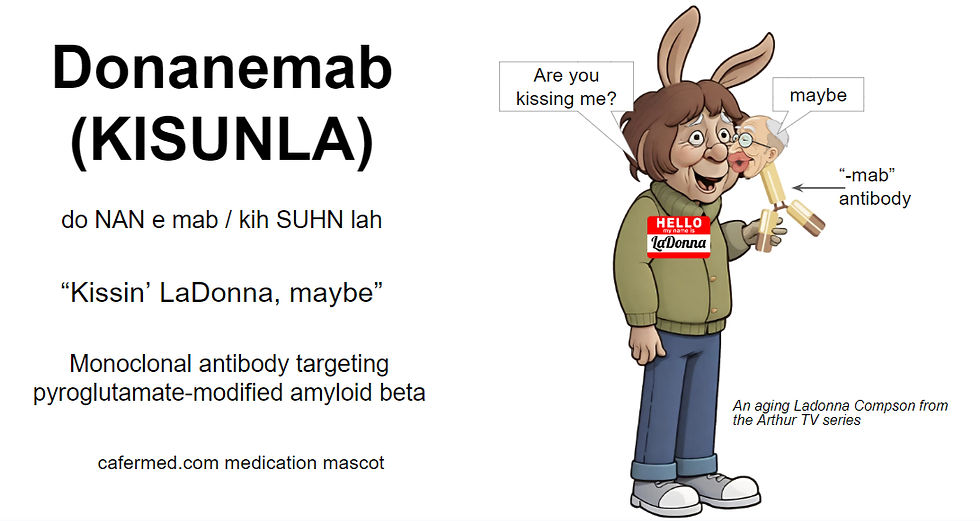
Donanemab (KISUNLA)
Pronunciation: do NAN e mab (kih SUHN lah)
Mascot: "Kissin' LaDonna, maybe"
FDA-approved for:
Mild cognitive impairment with evidence (PET scan) of amyloid beta pathology
Mild Alzheimer’s dementia
Mechanism
Donanemab (Kisunla) is a monoclonal antibody approved in 2024 for the treatment of Alzheimer's disease in people with mild cognitive impairment or mild dementia. The binding of an antibody to amyloid beta (Aβ) tags Aβ for removal by microglia, the brain’s resident immune cells. This process is called opsonization, which literally means "to buy food,” involving microglia “eating” Aβ.
Donanemab is the third antibody against amyloid beta (Aβ) to come to market, following aducanumab (removed from market) and lecanemab (Leqembi). Accumulation of Aβ may begin 20 years or more before symptoms arise (Vermunt et al., 2019). Aβ exists in various forms, including monomers, oligomers, and plaques. The potential advantage of donanemab is that it specifically targets N-terminally pyroglutamate-modified amyloid β proteins (abbreviated as Aβp3-x or N3pG).
The N3pG (pyroglutamate) form of Aβ is particularly harmful. Compared to unmodified Aβ, pyroglutamate-modified Aβ, also referred to as insoluble N-terminally truncated Aβ, has a higher tendency to aggregate into plaques and is more resistant to enzymatic degradation.
Donanemab is administered as a monthly intravenous infusion given over approximately 30 minutes. It was tested for up to 72 weeks in clinical trials. It is a humanized immunoglobulin gamma 1 monoclonal antibody. The full generic name of the medication is donanemab-azbt. The four-letter suffix has no pronunciation or meaning. Such suffixes are added to biologic drugs to distinguish reference products from their biosimilars. The suffix "-mab" is used for monoclonal antibodies.
Indication
The FDA approval was based on studies of donanemab in adults aged 59 to 86 years with confirmed amyloid pathology by PET scan and mild cognitive impairment or mild dementia.
Mild Cognitive Impairment (MCI) specifically refers to a stage of cognitive decline that is noticeable and measurable but not severe enough to interfere significantly with daily life and routine activities. Individuals with MCI do not have dementia and may not necessarily progress to dementia. In other words, donanemab is approved for Stage 3 and Stage 4 of the Global Deterioration Scale (GDS).
Stage 1: No Impairment (Normal Function)
Stage 2: Very Mild Cognitive Decline (Age-Associated Memory Impairment / Subjective Memory Loss)
Stage 3: Mild Cognitive Impairment ~ “Pre-dementia”
Stage 4: Moderate Cognitive Decline (Mild or Early-Stage Dementia)
Stage 5: Moderately Severe Cognitive Decline (Moderate Dementia)
Stage 6: Severe Cognitive Decline (Moderately Severe Dementia)
Stage 7: Very Severe Cognitive Decline (Severe or Late-Stage Dementia)
Participants were also required to have gradual and progressive change in memory function for at least 6 months and a Mini-Mental State Examination (MMSE) score of 20 to ≤28 (out of 30).
Efficacy
In a Phase 2 clinical trial called TRAILBLAZER-ALZ, individuals who received donanemab showed a statistically significant reduction in the rate of decline in cognition and daily function compared to placebo.
The effect size was small, as visualized by by Espay, Kasper, & Herrup (2024). According to their interpretation, the magnitude of functional improvement seen with donanemab is below the threshold for clinical importance.
The study allowed for cessation of donanemab dosing guided by amyloid PET levels measured at 24, 52, and 76 weeks if the amyloid plaque level was <11 Centiloids on a single PET scan or 11 to <25 Centiloids on two consecutive PET scans. At Weeks 24, 52, and 76, the proportion of participants in the donanemab treatment arm who met dose stopping criteria based on amyloid PET results was 17%, 42%, and 60%, respectively.
Risks and Side Effects
Donanemab accelerates loss of brain volume. Cognitively impaired participants treated with anti-Aβ drugs, donanemab included, are projected to regress toward brain volumes typical of Alzheimer dementia ∼8 months earlier than if they were untreated (Alves et al, 2023).
As with other anti-Aβ antibodies, donanemab can cause amyloid-related imaging abnormalities (ARIA), including ARIA with edema (ARIA-E) and ARIA with hemosiderin deposition (ARIA-H). ARIA is usually asymptomatic, although ARIA-E can cause focal neurologic deficits that can mimic ischemic stroke. Serious intracerebral hemorrhages >1 cm have occurred in patients treated with this class of medications.
Individuals who are ApoE ε4 homozygotes (those with high risk of developing Alzheimer’s disease at a younger age) have a higher incidence of ARIA. Testing for ApoE ε4 status should be performed prior to initiation of treatment to inform the risk of developing ARIA.
Incidence of ARIA
Symptomatic ARIA occurred in 6% (52/853) of patients. Symptoms associated with ARIA resolved in approximately 85% (44/52) of patients.
Including asymptomatic radiographic events, ARIA was observed in 36% (307/853) of patients treated with donanemab, compared to 14% (122/874) of patients on placebo.
ARIA-E (edema) was observed in 24% (201/853) of patients treated with donanemab compared with 2% (17/874) of patients on placebo.
ARIA-H (hemosiderin) was observed in 31% (263/853) of patients treated with donanemab compared with 13% (111/874) of patients on placebo.
Incidence of Cerebral Hemorrhage
Intracerebral hemorrhage greater than 1 cm in diameter was reported in 0.5% (4/853) of patients after treatment with donanemab, compared to 0.2% (2/874) of patients on placebo.
Death
According to the prescribing information, one fatal intracerebral hemorrhage occurred in a patient taking donanemab in the setting of focal neurologic symptoms of ARIA and the use of a thrombolytic agent. FDA staff noted that overall there were 17 deaths in patients given donanemab, compared with 10 who received placebo.
Summary of Intracerebral Events
No more than 1.4% (12/853) of patients experienced potentially irreversible intracerebral events.
Infusion-Related Reactions
Infusion-related reactions were observed in 9% (74/853) of patients treated with donanemab, mostly mild (57%) or moderate (39%). Infusion-related reactions resulted in discontinuations in 4% (31/853) of patients. Infusion-related reactions may consist of chills, erythema, nausea/vomiting, difficulty breathing/dyspnea, sweating, elevated blood pressure, headache, chest pain, and low blood pressure. 0.5% of patients receiving placebo experienced a reaction.
If an infusion reaction occurs, pre-treatment with antihistamines, acetaminophen, or corticosteroids prior to subsequent dosing may be considered.
Hypersensitivity Reactions
Hypersensitivity reactions, including anaphylaxis, occurred in 3% of patients (vs. 0.7% placebo).
Gastrointestinal Events
Three patients (0.4%) experienced intestinal obstruction (vs. 0% placebo). Two patients (0.2%) experienced intestinal perforation (vs. 0.1% placebo).
Bacteria populating the GI tract can release significant amounts of amyloids. As a side note, it has been hypothesized that the composition of gut microbiota may be a modifiable risk factor for the onset of Alzheimer’s disease (Pistollato et al., 2016). Nutritional interventions might prove to be an effective strategy to prevent or reduce the risk of dementia.
Other Side Effects
13% of patients experienced a headache (vs. 10% with placebo).
Overall Discontinuation
13% of patients treated with donanemab stopped treatment because of an adverse reaction, compared to 4% with placebo.
Cost
About $2,666 monthly. According to the manufacturer Lilly, coverage for Kisunla is available for eligible patients on Medicare.
Pharmacodynamic Interactions
Caution with antithrombotic or thrombolytic agents that could potentially increase risk of cerebral hemorrhage.
Pharmacokinetic Interactions
None
Dosing and Monitoring
700 mg IV monthly for the first 3 doses, and then 1400 mg monthly. Obtain an MRI prior to the 2nd, 3rd, 4th, and 7th infusions to screen for ARIA. Amyloid positron emission tomography (PET) levels are measured at weeks 24, 52, and 76. Prescribers can consider stopping treatment based on the reduction of amyloid plaques to minimal levels. Dosing can continue at the current dose and schedule if radiographically observed ARIA-E (edema) on MRI is mild and the patient is asymptomatic. If ARIA-E severity is mild and symptoms are mild (discomfort noticed, but no disruption of normal daily activity), dosing may continue based on clinical judgment. For moderate ARIA-E or moderate symptoms, treatment should be suspended. Dosing should be suspended for moderate ARIA-H (hemosiderin) or symptomatic ARIA-H of any severity.
Amyloid Controversy
But how effective is donanemab really, and will it have a clinically meaningful disease-modifying impact? This is a controversial topic.
There has been a long-prevailing theory that pathological (disease-defining) Aβ proteins are pathogenic (disease-causing). Some researchers feel the theory has been essentially disproven. Daly, Herrup, & Espay (2022) asserted that human trials of amyloid-lowering therapies should be abandoned due to futility. They cite 40 failed trials of amyloid-lowering therapies over the past two decades, many of which succeeded in lowering amyloid as designed.
A minority opinion was articulated by Karl Herrup (2021):
Hardy and Higgins (1992) presented the amyloid cascade hypothesis: amyloid plaques and neurofibrillary tangles (tau protein) might cause Alzheimer’s disease.
If plaques and tangles cause Alzheimer’s disease, then their constituents [aggregated Aβ and/or tau] must be neurotoxic.
It is true that Aβ and tau are neurotoxic. This is consistent with the amyloid cascade hypothesis but not proof.
Most data tend to falsify the hypothesis, yet it persists, indeed dominates, not as hypothesis but as dogma.
We have added tau and amyloid to the brains of healthy mice and humans (??), yet the predicted onslaught of Alzheimer’s disease either does not occur or occurs so slowly that we should search for other, perhaps more direct causes.
We have removed Aβ and tau from the brains of people with Alzheimer’s disease (with antibodies such as donanemab), yet they continue their cognitive decline.
We still debate whether the decline is less steep than in untreated persons, but under even the most optimistic readings of the data, the effect of removing amyloid or tau is modest.
“Our field lacks the courage to answer one simple question: what experimental result could we agree on that would falsify the amyloid cascade hypothesis? If the answer is ‘none,’ then it is dogma.”
Regarding pharmaceutical industry scientists—”It is hard to make a person understand something if their salary depends on their not understanding it.”
Amyloid-reducing antibodies, even those found to improve functioning—donanemab included—accelerate loss of brain volume.
Controversy Surrounding Donanemab Specifically
The clinical trial employed brain tau PET imaging as an enrichment strategy to increase the proportion of participants who were likely to progress during the placebo-controlled period. Subjects with no or very low tau were excluded from the placebo-controlled trial, but were eligible to enroll in a safety trial that did not involve clinical efficacy assessments. In the placebo-controlled trial, low/medium tau subjects were prioritized (over high tau subjects) in the statistical analysis. Despite this, the manufacturer (Lilly) did not propose a requirement for quantification of tau pathology in the prescribing information. There were no notable differences in safety between individuals with very low or no tau and individuals with higher tau burden. An independent report advised the FDA that it may be reasonable to generalize the efficacy results across the spectrum of tau burden. So this is probably a non-issue.
The primary endpoint was the change from baseline in the integrated Alzheimer’s Disease Rating Scale (iADRS) at 76 weeks. The study was initially designed with the CDR-SB as the primary endpoint but was changed during the conduct of the study. In the meeting minutes from 2021, the FDA Division of Neurology stated that, “we do not agree that a statistically significant treatment effect on the iADRS, unaccompanied by a valid statistically significant treatment effect on its two components, is acceptable for use as a primary efficacy assessment. Thus, the iADRS should not be used as your primary efficacy assessment.” The Division reiterated its concerns with the use of the iADRS as the primary endpoint at a 2022 meeting. Although the Agency had disagreed with the use of the iADRS as the primary endpoint, the statistically significant results of iADRS were supported by statistically significant results of its two component scores. So this also appears to be a non-issue.
My Take on Donanemab
This infographic highlights the key points. Donanemab is effective at clearing amyloid, but the clinical benefits are minimal. This implies that simply clearing amyloid may not be the solution, or that any potential benefits are offset by neurotoxicity, as indicated by accelerated brain volume decline. Hopefully, future treatments will reduce amyloid deposits while preserving brain volume.
Copyright 2024 CaferMed Publishing, Intended for prescribers
Comments